Bipolar affective disorder
Diagnostics According to ICD-10 V F31.3
International Classification of Psychological Disorders ICD-10 Chapter V.
– bipolar affective disorder, currently moderate depressive episode F31.3
(Dilling et. al. 2011).
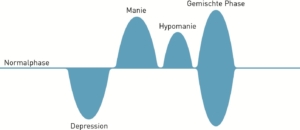
As Kasper and Hauk (2006) have described, the bipolar affective disorder shows three manifestations. These are differentiated by their different mood bases. The first phase is called low phase depression, the second mania/hypomania, and the third phase the normal phase, in which there is neither a manic nor a depressive phase. This mood can come and go regardless of the time or extent of each other. That is why assigning this disease is complicated. The course of these forms is characterized by two different alternating phases. A depressive current mood and the other one the high phase/ mania. An appearance can also be a mixture of both phases.
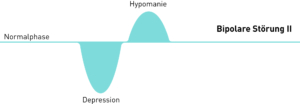
This progressive form is characterized by a change of at least one depressive phase, with a subsequent strong high phase (mania) or a mixed form of both phases (ibid.).
The schematic illustration shows an overview of the different disturbance phases
Fig.8: Individual phases of the bipolar disease.
Source: (Kasper & Hauk 2006)
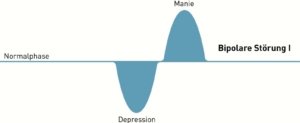
If the euphoric phase lasts at least 14 days, this process can be called mania. However, it is not said that the patient had depression before. This still does not mean that it is crucial for mania.
Fig.9: Bipolar disease phase II.
Source: (Kasper & Hauk 2006:12)
Fig.10: Bipolar disorder phase III.
Source: (Kasper & Hauk 2006:13)
Therapy
As Ebert and Loew (2011) describe it, bipolar disorder requires drug treatment that will certainly take a long time, while relapse prophylaxis is unavoidable as long-term therapy. These measures should be started within one year after the symptoms have subsided. In the event of a relapse, the therapies are repeated. The episodes can be reduced and a permanent absence of symptoms is achieved (ibid.).
Depression is treated with psychotropic drugs and antidepressants. As already stressed by Frank (2007), it is also recommended to take advantage of psychotherapy, but this only makes sense after the acute phase. In the acute episode an inpatient stay is necessary to ensure intensive therapy and to avert the risk of suicide. In the case of mild forms, outpatient treatment is often sufficient, especially if reliable relatives monitor the patient. The patient himself should not expose himself to any occupational stress – not even road traffic (ibid.).
Once the diagnostic criteria have been met, it is important that internal and neurological examinations begin. As already described by Laux, the blood count is determined in the laboratory (liver, kidneys, electrolytes, blood sugar, cal, thyroid values, vitamin B12 levels, serum iron levels), EEG, CT, possibly NMR, brain scintigraphy, SPECT, rCBF, Doppler sonography follow. A dexamethasone test should be performed in the event of a remission of depression. Standardized evaluation scales facilitate the evaluation of the severity of the disease (Laux 2001)
.
Bipolar affective disorder related to disease progression
At the time of explaining the bipolar affective disorder in the patient, it was clear that her condition was restless. She indicated a strong inner restlessness, which was also expressed in a clear motor restlessness, whereby she often got up from the armchair during the anamnesis and walked up and down in the room. Her thoughts were accelerated, verbose, and sometimes she jumped from one thought to another. Her concentration and memory function were significantly reduced. The mood varied greatly between euphoria and irritation. She reported sleeping disorders, with the subjective feeling that she needed less sleep lately.
In the last few months the patient had not taken her medication regularly, which led to another outbreak of a manic phase.
After also several depressive phases were explodeable and known, the diagnosis of the bipolar affective disorder, presently moderate depressive episode F31.3, was established.
Univ. Prof. DR. Andrawis